Health Library
Hemolytic-uremic syndrome
HUS; STEC-HUS; Hemolytic-uremic syndrome
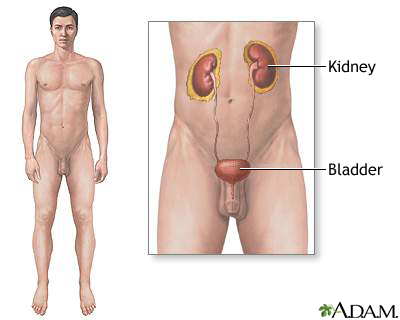
Shiga-like toxin producing E coli hemolytic-uremic syndrome (STEC-HUS) is a disorder that most often occurs when an infection in the digestive system produces toxic substances. These substances destroy red blood cells and cause kidney injury.
Images
I Would Like to Learn About:
Causes
Hemolytic-uremic syndrome (HUS) often occurs after a gastrointestinal infection with E coli bacteria (Escherichia coli O157:H7). However, the condition has also been linked to other gastrointestinal infections, including shigella and salmonella. It has also been linked to non-gastrointestinal infections.
HUS is most common in children. It is the most common cause of acute kidney failure in children. Several large outbreaks have been linked to undercooked hamburger meat contaminated with E coli.
E coli can be transmitted through:
- Contact from one person to another
- Consuming uncooked food, such as milk products or beef
STEC-HUS is not to be confused with atypical HUS (aHUS) which is not infection-related. It is similar to another disease called thrombotic thrombocytopenic purpura (TTP).
Symptoms
STEC-HUS often begins with vomiting and diarrhea, which may be bloody. Within a week, the person may become weak and irritable. People with this condition may urinate less than normal. Urine output may almost stop.
Red blood cell destruction leads to symptoms of anemia.
Early symptoms:
Later symptoms:
- Bruising
- Decreased consciousness
- Low urine output
- No urine output
- Pallor
- Seizures -- rare
- Skin rash that looks like fine red spots (petechiae)
Exams and Tests
Your health care provider will perform a physical exam. This may show:
- Liver or spleen swelling
- Nervous system changes
Laboratory tests will show signs of hemolytic anemia and acute renal failure. Tests may include:
- Blood clotting tests (PT and PTT)
- Comprehensive metabolic panel may show increased levels of BUN and creatinine
- Complete blood count (CBC) may show increased white blood cell count and decreased red blood cell count
- Platelet count is usually reduced
- Review of a blood smear, which shows deformed and fragmented red blood cells
- Urinalysis may reveal blood and protein in the urine
- Urine protein test can show the amount of protein in the urine
Other tests:
- Stool culture may be positive for a certain type of E coli bacteria or other bacteria
- Colonoscopy
- Kidney biopsy (in rare cases)
Treatment
Treatment may involve:
- Dialysis
- Medicines, such as corticosteroids
- Management of fluids and electrolytes
- Transfusions of packed red blood cells and platelets
Outlook (Prognosis)
This is a serious illness in both children and adults, and it can cause death. With proper treatment, more than half of people will recover. The outcome is better in children than adults.
Possible Complications
Complications may include:
- Blood clotting problems
- Hemolytic anemia
- Kidney failure
- Hypertension leading to seizures, irritability, and other nervous system problems
- Too few platelets (thrombocytopenia)
- Uremia
When to Contact a Medical Professional
Contact your provider if you develop symptoms of HUS. Emergency symptoms include:
- Blood in the stool
- No urination
- Reduced alertness (consciousness)
Contact your provider if you have had an episode of HUS and your urine output decreases, or you develop other new symptoms.
Prevention
You can prevent the known cause, E coli, by cooking hamburger and other meats well. You should also avoid contact with unclean water and follow proper hand washing methods.
Related Information
Acute kidney failureHemolytic anemia
Thrombocytopenia
Thrombotic thrombocytopenic purpura
Hemolysis
Anemia
Paleness
Chronic kidney disease
Prerenal azotemia
References
Alexander T, Licht C, Smoyer WE, Rosenblum ND. Diseases of the kidney and upper urinary tract in children. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap: 72.
George G, Friedman KD. Thrombotic thrombocytopenic purpura and the hemolytic uremic syndromes. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 132.
Mele C, Noris M, Remuzzi G. Hemolytic uremic syndrome. In: Ronco C, Bellomo R, Kellum JA, Ricci Z, eds. Critical Care Nephrology. 3rd ed. Philadelphia, PA: Elsevier; 2019:chap 50.
BACK TO TOPReview Date: 3/31/2024
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
